🌿 Irritable Bowel Syndrome (IBS): Friendly Guide to Symptoms, Causes & Relief – Internist geriatrician PCP Georgetown TX
- Dr. Mohammad Al Darawsha MD

- Aug 12, 2025
- 4 min read
IBS is common—and frustrating—but you’re not alone. With the right plan, most people feel much better. At Wellness Bay Primary Care, your Internist, geriatrician, and PCP in Georgetown TX, we’ll help you find triggers, calm symptoms, and get back to living comfortably.
What is IBS?
IBS is a functional gut disorder—meaning bowel movements and gut sensitivity are off, even though routine tests look normal. Symptoms tend to come and go and can be linked to food, stress, or hormones.
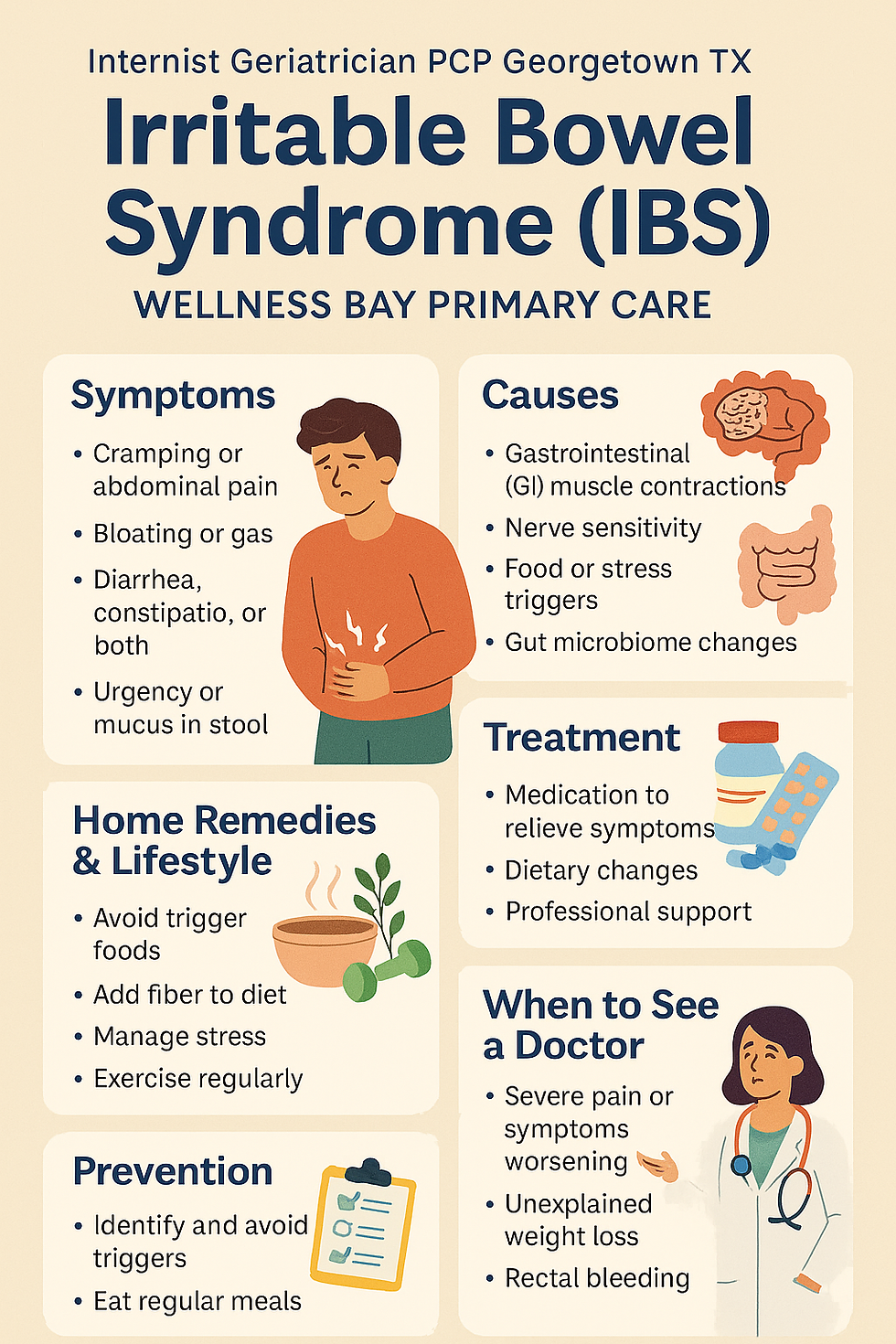
Common Symptoms
Cramping or abdominal pain (often better after a BM)
Bloating or gas
Diarrhea, constipation, or both (IBS‑D, IBS‑C, IBS‑M)
Urgency or the feeling you didn’t finish
Mucus in stool (not blood)
If you see blood, have fever, or unintentional weight loss, skip home care and contact us promptly.
Causes (Why IBS Happens)
IBS is usually a mix of factors:
Gut–brain communication changes (nerves become extra sensitive)
Altered motility (colon moves too fast or too slow)
Microbiome shifts after infection, antibiotics, or stress
Food triggers (e.g., high‑FODMAP foods, excess caffeine)
Stress, anxiety, or poor sleep (they don’t “cause” IBS but can magnify it)
Pathophysiology (In Simple Terms)
Think of the gut like a microphone turned up too loud:
Visceral hypersensitivity: normal gas/stretch feels painful.
Dysmotility: spasms speed things up (diarrhea) or slow them down (constipation).
Microbiome & bile acids: changes can drive gas, bloating, or loose stools.
Gut–brain axis: stress signals amplify gut nerves, creating a loop of symptoms.
Helpful Investigations (Personalized—not “one size fits all”)
Your plan may include:
Basic labs (CBC, CMP), celiac screen, thyroid (TSH)
Stool tests when appropriate (calprotectin, fecal pathogens)
Lactose intolerance or SIBO evaluation if suspected
Colonoscopy only when red‑flags or age‑based screening apply
We keep testing focused—enough to be safe, never excessive.
Treatment: Home Remedies, Lifestyle & Medical Options
Lifestyle & Home Strategies
Low‑FODMAP trial (2–6 weeks), then gentle re‑introductions
Psyllium fiber (start low, go slow) for IBS‑C/IBS‑M
Peppermint‑oil (enteric‑coated) for cramping/bloating
Steady meals, adequate hydration, limit alcohol/caffeine
Movement most days (even 20–30 min walks)
Stress support: breathing drills, mindfulness, CBT, or counseling
Sleep 7–9 hours; keep a simple symptom/food tracker
Medications (tailored to your subtype)
IBS‑D: loperamide as needed; bile‑acid binders; rifaximin course; low‑dose TCAs for pain/urgency
IBS‑C: osmotic laxatives (PEG), secretagogues (linaclotide, plecanatide), low‑dose SSRIs if pain + mood
Cramping: antispasmodics (e.g., dicyclomine) used thoughtfully
Bloating/gas: targeted probiotics (trial 4–8 weeks)
We’ll review interactions and pick the simplest plan that fits your life.
Prevention & Flare Control
Identify your personal trigger pattern (food, stress, sleep debt).
Keep fiber consistent day‑to‑day.
Plan “gentle eating” on high‑stress days.
Revisit your toolbox (peppermint oil, breathing, walk after meals).
When to See a Doctor (or Seek More Testing)
New or worsening symptoms after age 50
Red flags: rectal bleeding, black stools, fever, unintended weight loss, persistent night symptoms, anemia, family history of IBD/colon cancer
Severe pain, dehydration, or symptoms not improving with home care
You’d like a clear diagnosis and a simple, personalized plan
How We Help—Internist geriatrician PCP Georgetown TX
At Wellness Bay Primary Care, we provide:
A kind, unrushed visit to hear your story
Focused testing (only what’s needed)
A clear plan: food strategy, symptom‑calming tools, and meds only if helpful
Follow‑ups to tune your plan until you feel better
Top 10 FAQs (Quick & Friendly)
1) Is IBS dangerous?
No—uncomfortable, yes; dangerous, no. We still rule out other causes.
2) Can stress really flare IBS?
Yes; the gut–brain axis is real. Stress tools often reduce symptoms.
3) Do I need a colonoscopy?
Only if red flags or screening age/risk say so—we’ll guide you.
4) Which fiber is best?
Psyllium has the best evidence. Add slowly, hydrate well.
5) Are probiotics worth it?
Some strains help bloating/regularity. We do a timed trial and reassess.
6) What is low‑FODMAP?
A short, structured elimination to spot triggers—then re‑add foods you tolerate.
7) Can coffee cause flares?
For some. Try smaller amounts or switch to low‑acid/half‑caf.
8) Is peppermint oil safe?
Enteric‑coated capsules can reduce cramping; avoid if reflux worsens.
9) Will I need long‑term meds?
Often no. Many do well with lifestyle + “as‑needed” tools.
10) How fast will I feel better?
Many notice improvements in 2–6 weeks with a tailored plan.
💬 Let’s Keep You Healthy, Together
The Medicare Wellness Visit is your chance to pause, plan, and protect your future health. At Wellness Bay Primary Care, we make this visit meaningful, respectful, and centered on you.
📍 Visit us at 4887 Williams Dr Ste 107, Georgetown TX
📞 Call 512.588.7008 or📲 Book online
Proudly, our Internal Medicine Primary Care Practice is Accepting new patients From:
Georgetown, Sun City, Round Rock, Cedar Park, Leander, Liberty Hill, Florence, Jarrell, Taylor, Hutto, Pflugerville, North Austin, Brushy Creek, Temple, Harker Heights, Bartram, Lampasas, Killeen, Lago Vista, and surrounding areas across Williamson County and North Austin TX
📍 Related Links