Microscopic Colitis Care with an Internist Geriatrician PCP in Georgetown TX
- Dr. Mohammad Al Darawsha MD

- Aug 15, 2025
- 3 min read
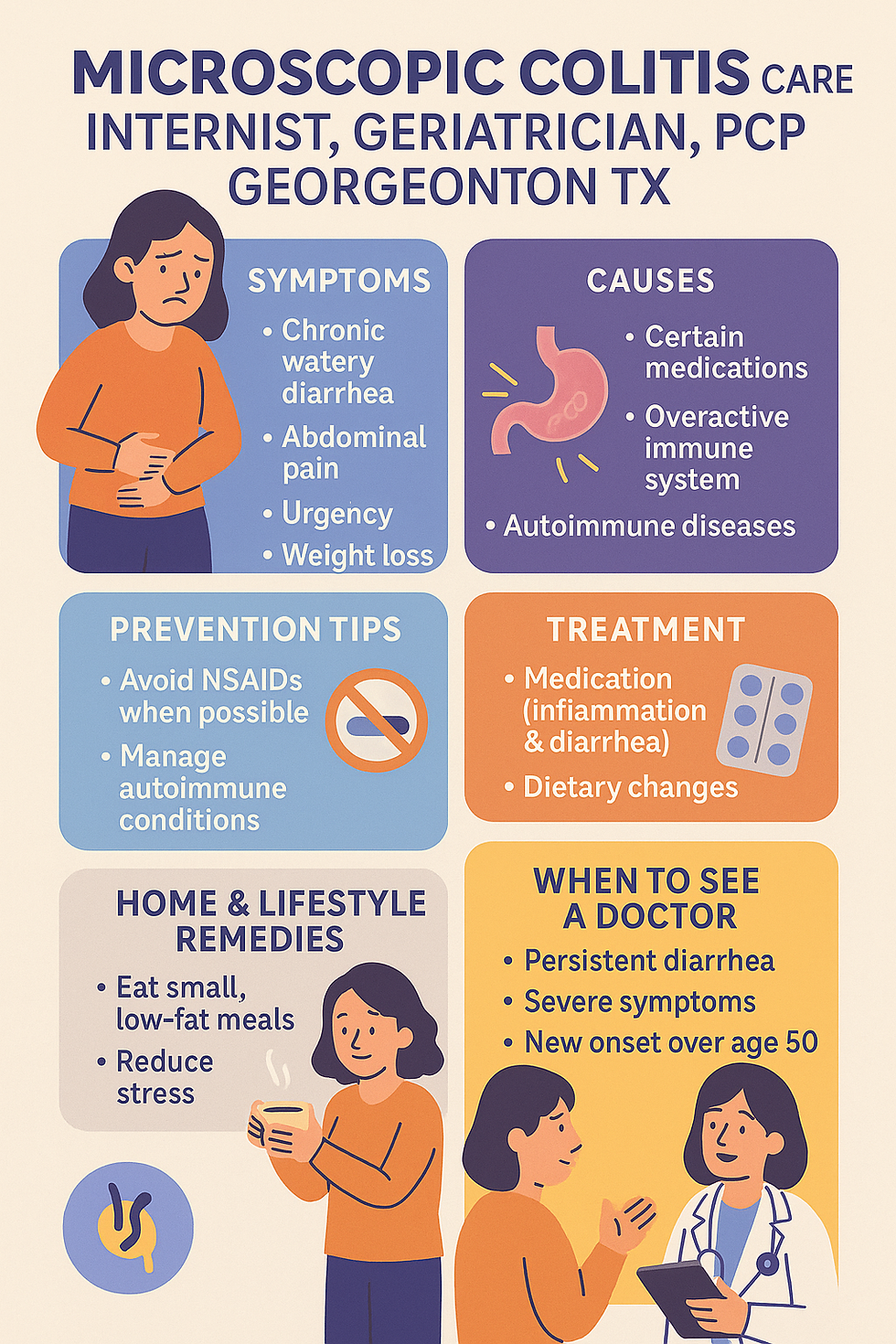
Microscopic colitis is a condition that causes chronic, watery diarrhea—often without blood—and can greatly affect daily comfort. The good news? It’s manageable, and you don’t have to face it alone. At our clinic in Georgetown TX, our internist, geriatrician, and PCP team offers compassionate, unrushed visits to help you understand your symptoms, find the cause, and guide you toward relief.
Causes of Microscopic Colitis
The exact cause isn’t always clear, but several factors may contribute:
Overactive immune response in the colon
Certain medications (NSAIDs, PPIs, SSRIs)
Autoimmune disorders (celiac disease, thyroid disease)
Infections or bacterial imbalance
Smoking or chronic irritation of the bowel lining
Symptoms
Chronic watery diarrhea (often multiple times a day)
Abdominal pain or cramping
Urgency to use the bathroom
Fatigue from frequent bowel movements
Mild weight loss in some cases
Pathophysiology (How It Works in the Body)
In microscopic colitis, the inner lining of the colon becomes inflamed at a microscopic level—meaning it looks normal during colonoscopy, but inflammation is seen under the microscope. This inflammation disrupts fluid absorption, causing persistent diarrhea.
Risk Factors
Age over 50 (more common in older adults)
Female gender
Autoimmune diseases
Long-term use of certain medications
Family history of bowel disorders
Prevention Tips by your Internist Geriatrician PCP in Georgetown TX
While it can’t always be prevented, you can lower your risk or reduce flare-ups by:
Avoiding unnecessary NSAIDs (like ibuprofen) and certain acid reflux meds if alternatives exist
Managing autoimmune diseases effectively
Staying hydrated and eating a gut-friendly diet
Quitting smoking
Investigations
To diagnose microscopic colitis, your doctor may recommend:
Colonoscopy with biopsies (the gold standard)
Stool tests to rule out infection
Blood tests for inflammation and autoimmune conditions
Treatment Options
Medical Treatments
Prescription anti-inflammatory medications (like budesonide)
Anti-diarrheal agents for symptom control
Stopping or switching medications that might trigger symptoms as advised by your Internist Geriatrician PCP in Georgetown TX.
Home & Natural Remedies
Eating smaller, more frequent meals
Avoiding trigger foods (spicy, fatty, high-lactose)
Limiting caffeine and alcohol
Increasing soluble fiber slowly (like psyllium husk)
Staying well-hydrated with electrolyte-rich fluids
Lifestyle Changes to Support Recovery
Stress reduction techniques (yoga, meditation, gentle walks)
Keeping a food diary to track symptom triggers
Maintaining a balanced diet with whole foods
Working with your PCP for medication review
When to See a Doctor
Visit your PCP in Georgetown TX if you experience:
Persistent watery diarrhea for more than 2 weeks
Unexplained weight loss
Blood in stool
Severe dehydration symptoms (dizziness, weakness, confusion)
New bowel changes over age 50
Top 10 FAQs About Microscopic Colitis
(SEO-optimized & patient-friendly)
Is microscopic colitis the same as ulcerative colitis?No — it’s a different condition, usually milder, and only seen under the microscope.
Can microscopic colitis go away on its own?Sometimes, but many cases need treatment to avoid long-term symptoms.
What foods should I avoid?Spicy foods, high-fat meals, caffeine, and artificial sweeteners can worsen symptoms.
Does stress make it worse?Yes, stress can trigger flare-ups in some people.
Is it contagious?No — it’s not spread from person to person.
Can I still eat fiber?Yes — soluble fiber may help, but introduce it gradually.
Do probiotics help?They may help restore gut balance, especially after flare-ups.
Can medications cause it?Yes — NSAIDs, certain antidepressants, and reflux medicines may trigger it.
Do I need a colonoscopy?Yes — to confirm the diagnosis and rule out other conditions.
Will I have it for life?It can be chronic, but with the right treatment, many patients live symptom-free.
💬 Let’s Keep You Healthy, Together
The Medicare Wellness Visit is your chance to pause, plan, and protect your future health. At Wellness Bay Primary Care, we make this visit meaningful, respectful, and centered on you.
📍 Visit us at 4887 Williams Dr Ste 107, Georgetown TX
📞 Call 512.588.7008 or📲 Book online
Proudly, our Internal Medicine Primary Care Practice is Accepting new patients From:
Georgetown, Sun City, Round Rock, Cedar Park, Leander, Liberty Hill, Florence, Jarrell, Taylor, Hutto, Pflugerville, North Austin, Brushy Creek, Temple, Harker Heights, Bartram, Lampasas, Killeen, Lago Vista, and surrounding areas across Williamson County and North Austin TX
📍 Related Links